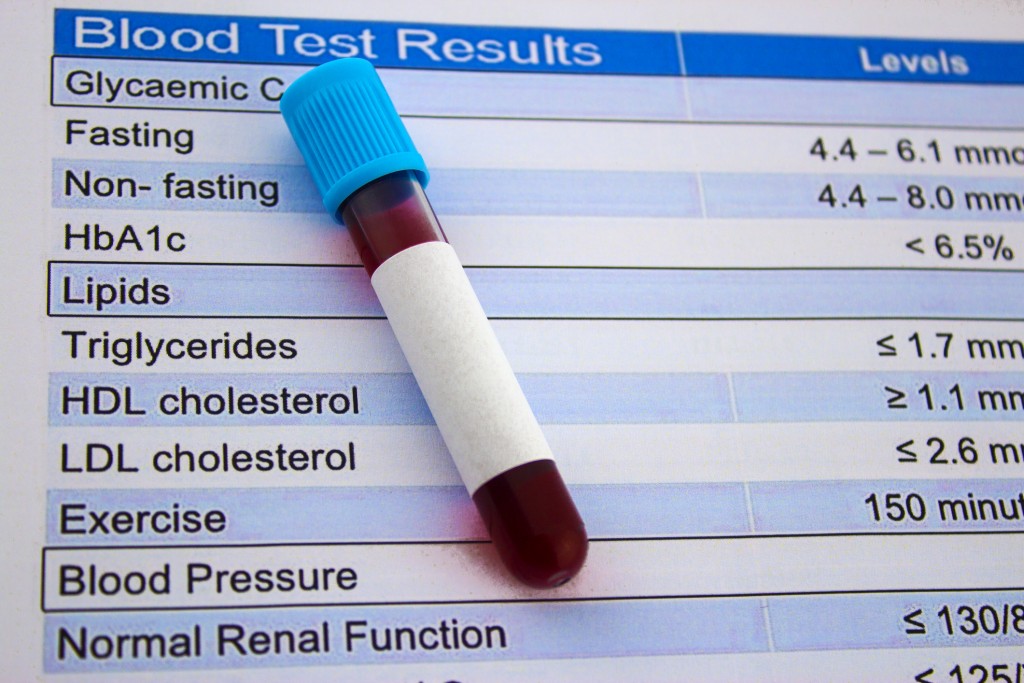
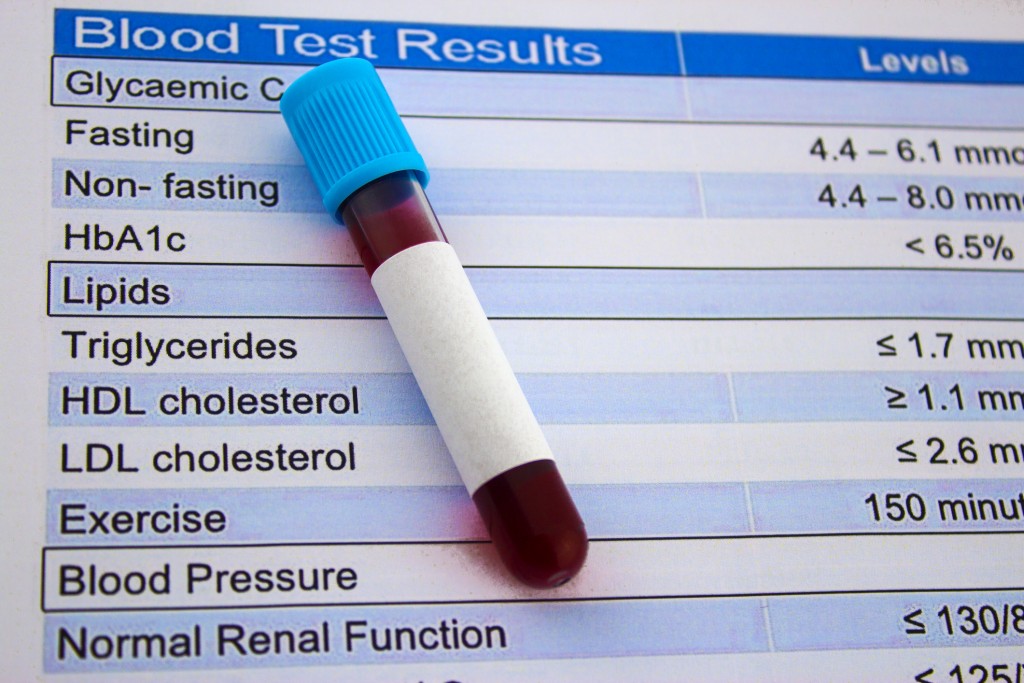
 Doctors often order a lipid panel as part of routine blood work during a physical examination. This test assesses a patient’s risk of developing cardiovascular disease, which includes heart attacks and strokes. Lipids are fats and fatty-like substances found in the blood. Cholesterol is one such fat. People who have high cholesterol levels are more likely to develop heart disease. A lipid panel measures cholesterol levels and helps the physician determine whether any treatment or lifestyle changes are necessary.
Doctors often order a lipid panel as part of routine blood work during a physical examination. This test assesses a patient’s risk of developing cardiovascular disease, which includes heart attacks and strokes. Lipids are fats and fatty-like substances found in the blood. Cholesterol is one such fat. People who have high cholesterol levels are more likely to develop heart disease. A lipid panel measures cholesterol levels and helps the physician determine whether any treatment or lifestyle changes are necessary.
A person should fast for 9-12 hours before a lipid panel is done. This ensures that the blood work is not affected by any food that was recently eaten. Three cholesterol levels are reported in a lipid panel – total cholesterol, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C).
HDL-C – This type of cholesterol is often called good cholesterol. It takes excess cholesterol to the liver to be removed from the body. A level of 60mg/dL or higher is optimal, lowering a patient’s risk for heart disease. A level of 40mg/dL is low, showing an increase in risk for heart disease.
LDL-C – This type of cholesterol is known as bad cholesterol. It gets deposited as plaque on the walls of arteries, narrowing them and decreasing the blood flow. Doctors ideally want this number to be less than 100mg/dL. Levels higher than 100mg/dL may be considered elevated, borderline high, or high. A change of diet, exercise, weight loss, or cholesterol medication may be discussed with the patient as strategies to help them lower the bad cholesterol to a more normal level.
Total cholesterol – This is a measure of all cholesterol. For total cholesterol, a result of 200mg/dL or lower indicates normal levels. A result higher than 240mg/dL is considered high.
A lipid panel also measures triglycerides in the lipoprotein particles. High levels of triglycerides are associated with cardiovascular disease. A result of 150mg/dL or more is considered high. The same strategies used to lower bad cholesterol are also recommended for lowering triglycerides.
The American Heart Association recommends that adults ages 20 and older have a lipid panel every 4-6 years. Higher risk individuals with heart disease, diabetes, or a family history of high cholesterol should have their levels checked more often. An individual may have high cholesterol without knowing it, as there are often no symptoms.
 Cholesterol levels are measured by a blood test referred to as a lipid profile or lipid panel. The numbers are broken down into LDL (low density lipoprotein), which is “bad” cholesterol and HDL (high density lipoprotein), known as the “good” cholesterol. Most of the body’s cholesterol falls into the LDL category.
Cholesterol levels are measured by a blood test referred to as a lipid profile or lipid panel. The numbers are broken down into LDL (low density lipoprotein), which is “bad” cholesterol and HDL (high density lipoprotein), known as the “good” cholesterol. Most of the body’s cholesterol falls into the LDL category.
An overabundance of LDL cholesterol forms a build up of plaque along the walls of the blood vessels. This plaque, if thick enough, can block blood flow causing a heart attack. The lower the LDL number, the lower the risk of developing heart disease.
The high density lipoproteins absorb cholesterol and take it to the liver. It can then be flushed from the body before it can block the blood vessels. A higher HDL number on the lipid profile indicates a lower risk for heart disease.
An LDL number of 190 mg/dL or higher means a higher risk for heart disease. An HDL number less than 40 mg/dL for men and less than 50 mg/dL for women indicates higher risk. The lipid profile also measures triglycerides and gives the total cholesterol number. The doctor takes all these numbers into consideration when recommending treatment options. Diet and lifestyle changes may be recommended to try to reduce the risk, or the patient may be prescribed medication such as a statin drug. Lifestyle changes can include eating a healthy diet, losing weight, exercising regularly, and quitting tobacco use. The doctor will also consider the patient’s other risk factors including age, weight, gender, race, diet, and medical history.
Adults at average risk for heart disease should have a cholesterol test every five years, beginning at age 18. The doctor may recommend testing more often if the patient is overweight, smokes, has diabetes, is physically inactive, or has a family history of heart disease.
To learn more about your cholesterol levels, contact RMD Primary Care to schedule an appointment.
Triglycerides are a type of fat in the blood. Most people are familiar with cholesterol levels but may have less knowledge about how triglycerides affect their health. Triglycerides are stored in fat cells and released when the body needs energy between meals. When we eat more calories than our body can burn, the level of triglycerides can become too high. This can lead to serious health issues.
Anyone at any age can develop high triglyceride levels. However, there are certain risk factors unique to women. Triglycerides can be elevated during pregnancy, by using birth control pills with estrogen, and by hormone replacement therapy. Certain medications can also raise triglyceride levels.
 A high triglyceride level can increase the risk for heart disease and stroke. It can contribute to hardening and thickening of the walls of the arteries. High triglycerides can also lead to inflammation of the pancreas. There are often no visible symptoms of high triglyceride levels. Routine blood tests, usually done along with cholesterol testing, will determine triglyceride levels. These tests are sometimes called a lipid profile or lipid panel. A normal triglyceride level is measured at less than 150 mg/dL; high triglycerides are between 200-499 mg/dL; very high levels are 500 mg/dL and over.
A high triglyceride level can increase the risk for heart disease and stroke. It can contribute to hardening and thickening of the walls of the arteries. High triglycerides can also lead to inflammation of the pancreas. There are often no visible symptoms of high triglyceride levels. Routine blood tests, usually done along with cholesterol testing, will determine triglyceride levels. These tests are sometimes called a lipid profile or lipid panel. A normal triglyceride level is measured at less than 150 mg/dL; high triglycerides are between 200-499 mg/dL; very high levels are 500 mg/dL and over.
Lifestyle changes can sometimes lower triglyceride levels naturally. Healthy eating habits can make a big difference. Avoid foods that are high in saturated fats, trans fats, and sugary carbohydrates. Choose low fat dairy and lean meats. Eat fish twice a week. Choose whole grains and foods high in fiber. Foods rich in omega 3 fatty acids including salmon, tuna, kale, spinach, and brussel sprouts can help lower triglycerides. Other lifestyle changes that are beneficial include exercising more, losing excess weight, and decreasing alcohol use.
Your doctor can monitor triglyceride levels through regular checkups and routine blood work. If lifestyle changes have not been enough to keep triglycerides under control, medications can be prescribed.
 Doctors often order a lipid panel as part of routine blood work during a physical examination. This test assesses a patient’s risk of developing cardiovascular disease, which includes heart attacks and strokes. Lipids are fats and fatty-like substances found in the blood. Cholesterol is one such fat. People who have high cholesterol levels are more likely to develop heart disease. A lipid panel measures cholesterol levels and helps the physician determine whether any treatment or lifestyle changes are necessary.
Doctors often order a lipid panel as part of routine blood work during a physical examination. This test assesses a patient’s risk of developing cardiovascular disease, which includes heart attacks and strokes. Lipids are fats and fatty-like substances found in the blood. Cholesterol is one such fat. People who have high cholesterol levels are more likely to develop heart disease. A lipid panel measures cholesterol levels and helps the physician determine whether any treatment or lifestyle changes are necessary.