Who Should Have a Bone Density Scan?

A bone density scan assesses a person’s risk for osteoporosis, a disease that affects approximately 10 million Americans. Osteoporosis causes a loss of minerals from the bones, leaving them brittle and vulnerable to fractures. The condition becomes more common with age, and many people don’t know they have osteoporosis until they break a bone. Old bone breaks down more quickly than new bone can be made.
Osteoporosis can affect both women and men; however, it is a common women’s health issue. A bone density, or DEXA scan, is the imaging test that is used to diagnose osteoporosis. The National Institutes of Health recommends women have a bone density scan at age 65. Then they should be rescreened in 2-3 years, if their results are good. Some doctors may recommend women aged 64 and under receive a bone density scan after going through menopause, since reduced levels of estrogen is a risk factor for osteoporosis.
Many physicians don’t recommend a DEXA scan for men until age 70, unless they’ve had a vertebral bone fracture, osteopenia of the spine, other broken bones, or additional risk factors. The National Osteoporosis Foundation recommends a DEXA scan for anyone over age 50 who breaks a bone.
Risk Factors for Osteoporosis
The most common risk factors for developing osteoporosis are age, post-menopausal female, small body frame, and a family history of the condition. Some medications pose risk factors including long-term use of cortisone, prednisone, thyroid hormone medications, anti-seizure drugs, and some cancer drugs. People having primary hyperthyroidism are also at higher risk.
Common Bone Fractures
Those with osteoporosis most commonly fracture a wrist, hip, or spinal vertebrae. There is no cure for osteoporosis, but medications can help slow down the rate of bone loss. Periodic bone density scans help doctors monitor the progression of the disease and evaluate how well the osteoporosis medication is working.
Test Preparation
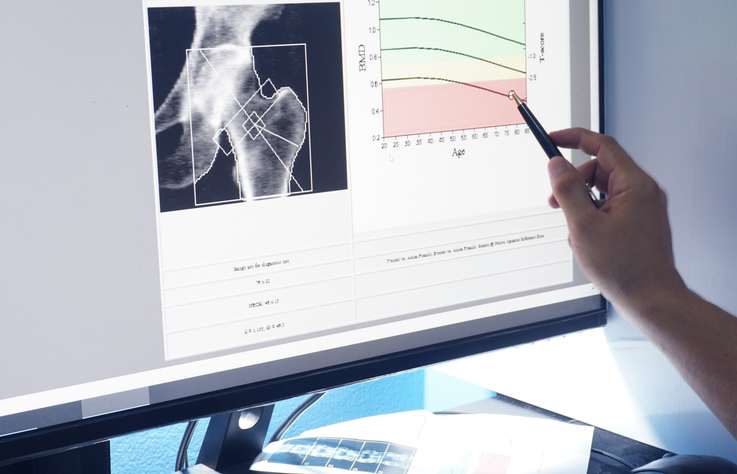
No special preparation is needed before a DEXA scan except to stop taking calcium supplements 24 hours before the test. The scan is a low dose x-ray that is totally painless. The patient will lie on their back on a padded table while the machine moves over the body. The entire process takes 15-30 minutes. The scan will be read by a radiologist, and a report is sent to the referring physician.
Will insurance pay for the test?
Medicare Part B covers a bone density scan for women once every 24 months, and more often if medically necessary. A person may qualify for more frequent tests if they have any of the following conditions, which could lead to decreased bone density:
- Rheumatoid arthritis
- Chronic kidney disease
- Overactive parathyroid gland or other hormonal imbalance
- Diabetes
- Organ transplant
Medicare will cover the test for men who have had a vertebral fracture or osteopenia of the spine. Many private health insurance companies also cover DEXA scans.
Next Steps
RMD Primary Care treats many common women’s health issues, such as osteoporosis. Our physicians can make a referral for a bone density scan. Contact our office to schedule an appointment.



















