B Vitamins and Women’s Health

B vitamins are vital in maintaining good health. They help promote a healthy metabolism, play a significant role in nerve function, help in the formation of red blood cells, and are linked to a reduced risk of stroke. Certain B vitamins are essential for normal brain development and for ensuring the immune system functions properly. Eight B vitamins make up the B Complex. All of them work together and are necessary for our well-being.
Importance for pregnant women

Vitamin B9 is essential during early pregnancy to prevent birth defects of the brain and spine. Doctors often prescribe a prenatal vitamin supplement to ensure women are getting enough. B vitamins can also help reduce PMS symptoms, reduce anxiety, improve mood, and improve memory.
B vitamins are water soluble, meaning they are not absorbed and stored in fat cells in the body. Excess amounts are eliminated in the urine. Many women don’t get enough B vitamins in their diet, although most are readily available in common foods.
The 8 B vitamins
Here are the eight B vitamins, ways the body uses them, and how to incorporate them into our diets.
B1 – (thiamin) Helps the body properly use carbohydrates. Found in whole grain cereal, nuts, beans, and meat.
B2 – (riboflavin) Necessary for normal cell growth and function; boosts the immune system. Found in eggs, dairy products, meat, nuts, and green vegetables.
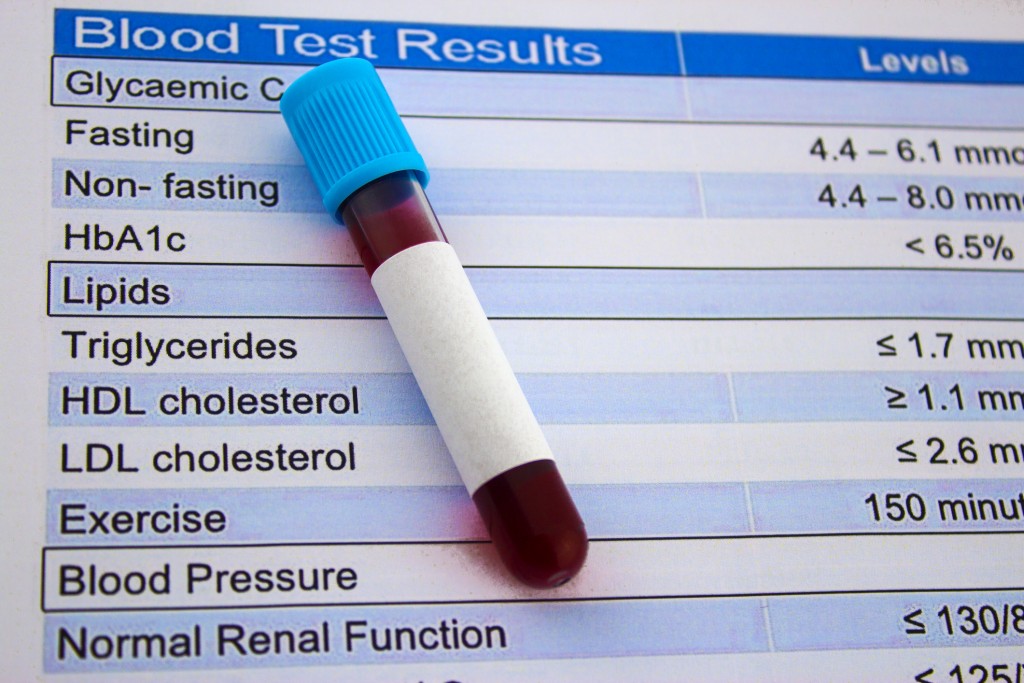
B3 – (niacin) Improves cholesterol levels; boosts good HDL and lowers triglycerides. Found in meat, poultry, fish, eggs, and greens.
B5 – (pantothenic acid) Necessary for hormone production; helps the body properly use carbs, proteins, and lipids. Found in organ meats, vegetables, cereal grains, eggs, dairy products, and legumes.
B6 – (pyridoxine) Necessary for proper growth and development of the brain, nerves, and skin; helps the body use sugars, fats, and proteins. Found in cereal grains, bananas, beans, spinach, lentils, eggs, and meat.
B7 – (biotin) Helps break down fats and carbs. Found in eggs, dairy products, and bananas.
B9 – (folate and folic acid) Involved in the production of genetic material, DNA. Found in leafy vegetables, okra, bananas, orange juice, and tomato juice.
B12 – (cyanocobalamin) Helps maintain healthy metabolism, blood cells, and nerves. Found in organ meats, beef, tuna, salmon, clams, sardines, and dairy products.
Vitamin B deficiency can result in symptoms that include anemia, fatigue, depression, eczema, hair loss, muscle cramps, and loss of appetite. Talk to the health care providers at RMD Primary Care to learn more about B vitamins and women’s health.