Should My College Student Get a Meningitis Vaccination?
 What is meningitis?
What is meningitis?
According to the Centers for Disease Control and Prevention (CDC), meningitis is an inflammation or swelling of the protective membranes covering the brain and spinal cord. Although meningitis can have several causes, the most common types are caused by bacteria and viruses. Outbreaks of some types of meningococcal disease have been reported on college campuses in recent years. Many states now require that incoming college students be vaccinated against meningococcal disease, particularly those who will be living in campus housing. The CDC highly recommends the vaccinations. It is considered preventative health.
Viral Meningitis
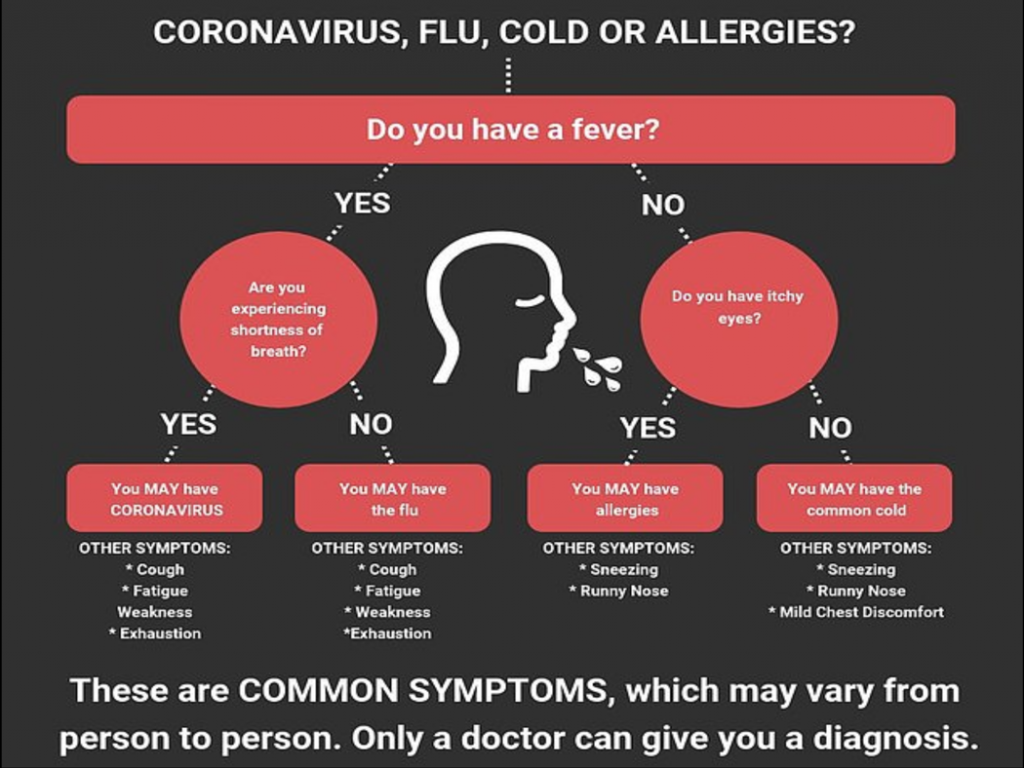
The most common type of meningitis is caused by viruses. While these infections are serious, they are usually less severe than bacterial meningitis. Early symptoms may seem like flu. There may be a high fever, stiff neck, severe headache, vomiting, seizures, confusion, sleepiness or difficulty waking from sleep.
Bacterial Meningitis
Symptoms are generally the same as the viral type. However, the onset of symptoms is very rapid. Bacterial meningitis can be life threatening. Swelling of the tissues around the brain can lead to paralysis, stroke, and death.
Meningitis diagnosis and treatment
Testing for meningitis is done through blood samples, nasal or throat swabs, and the drawing of spinal fluid for examination. There is no specific treatment for viral meningitis. Antibiotics are not used. Some antiviral medications may be effective. Most patients with mild cases will be able to recover on their own.
Patients with bacterial meningitis must receive immediate treatment with intravenous antibiotics. Sometimes corticosteroids are given to reduce brain swelling. If not treated quickly enough, a patient may develop sepsis and can die. Bacterial meningitis can cause permanent disabilities including hearing loss and brain damage.
Meningitis Vaccines for meningococcal disease
The CDC recommends that preteens ages 11-12 years old receive the MenACWY vaccine. This vaccine protects against four different strains of meningococcal bacteria. A booster dose should be given at age 16. Teens and young adults ages 16-23 may also get a MenB vaccine. The preferred age is 16-18 years, and multiple doses give the best protection. This vaccine protects against a less common strain of meningococcal disease. If your teenager has not received these vaccines, talk to your healthcare provider at RMD Primary Care about getting vaccinated.